
Bone Fracture Recovery Protocol: Nutrition & Supplement Considerations
In this article we are going to look at how nutrition can help optimize recovery from a bone fracture. We have used similar tactics outlined in this article to help stunt performers recover well from injury when the unexpected happens.
You will recover without this intervention; however, we have seen a number of remarkable and accelerated recovery times in those we have been able to support with nutrition and other injury acceleration techniques.
Understanding the fracture healing journey
Following a fracture there is a predictable healing journey. The more we know about the steps of recovery the more we can use nutrition to support the natural healing process.
Phase 1 – The inflammation phase
This is the first stage of fracture healing and recovery. After the initial fracture, the damaged cells at the edge of the fracture die back and release inflammatory chemicals known as cytokines, which initiate the healing process, this is why inflammation is a crucial part of the healing process.
Once the injury occurs blood-clotting forms, inflammation begins, clean-up cells are sent to the wounded area. The mesh of clotted blood is actually the first link between the fractures.
Repair cells are then sent directly to the fracture gap and immediately they begin the repair process.
An acute inflammatory reaction is a natural and critical response, usually lasting around 5 days post fracture. Although it is painful we need the inflammatory process for repair.
If we try to suppress the natural inflammatory reaction this may delay the recovery. Of course, chronic levels of inflammation should be addressed and after the initial 5day acute period after the injury or surgery, specific anti-inflammatory nutrient compounds can be used.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) in the case of bone fracture, should also be avoided if at all possible, as NSAIDs have been shown to be a risk factor for bone healing impairment, not to mention their often-negative impact on digestive health.
Phase 2 – Soft callus formation
Only a few days post fracture your body begins to lay down cartilage and fibrocartilage. This spongy material fills the gap between the fracture sites. It remains very weak at this point and therefore it is crucial to be very protective of the injury and in some cases, casts will be used to protect the site and limit the movement.
After just a couple of weeks the soft callus provides a site for new blood vessels to form and specific cells known as osteoblasts begin laying down woven bone, which becomes the first contact between the fracture sites.
This new bone substance eventually hardens, turning into what is known as hard callus.
Phase 3 – Hard callus formation
The subsequent 6-12 weeks after the formation of the soft callus, the body will completely turn the soft callus and the hard callus into woven bone. Weight bearing activities play a crucial role in stimulating the transformation from soft callus to hard callus and underlines the importance of a well-established and controlled exercise program as part of the rehab.
Phase 4 – Bone remodeling
The final stage is known as the remodeling phase. This is when the callus begins to mature and remodel itself. Specific cells remodel the newly woven bone after a collagen matrix becomes mineralized, thus creating the stronger bone.
The body initially lays down excessive amounts of hard callus than is required and this may be why on a follow up x-ray the site can look larger than other areas of the bone. However, over time the osteoblasts and osteoclasts begin to lay down and remove bone from where necessary, which can restore the normal shape of the bone.
Weight bearing exercise is a must during the remodeling phase, as it will lead to increased bone strength.
Specific Nutrition Considerations
Below are some of the key factors when it comes to using nutrition to support bone formation and assist the predictable fracture repair process.
1. Ensure you are eating enough calories
After a significant injury like a fracture, usually comes a period of immobility. The natural response can be to eat less, whereas during a fracture or any other acute injury for that matter, your body will require a surprisingly high demand for calories still. The more significant the injury the more calories that will be demanded to support the healing process.
You don’t need to count but you may have to override slightly your appetite which will likely drop if you are less active than normal.
You may want to use liquid nutrition to help overcome the lowered appetite caused by inactivity. Click the image below to download our simple smoothie formula.
2. Focus on anti-inflammatory foods to help reduce chronic inflammation
Chronic inflammation has the potential to slow the recovery process. Fortunately, there are many foods that can help lower inflammatory levels.
Some of your most anti-inflammatory based foods include:
- Omega-3 fats from oily fish, such as sardines, mackerel, herring, salmon (wild), trout (wild)
- Walnuts
- Flax and Pumpkin Seeds
- Olive oil (not heated)
- All colourful fruits and vegetables
- Turmeric and Ginger
As well as that I recommend certain natural anti-inflammatory and wound healing foods as well, these include:
Turmeric Milk
The extract from turmeric and ginger known as curcumin possesses anti-inflammatory capabilities. To allow it to go systemic and not just have a local anti-inflammatory effect in the gut, black pepper should be added to allow for increased absorption of the curcumin.
See recipe below (Add some black pepper):

Ingredients
- 2 cups milk (cashew/almond/coconut)
- 1 tsp ground turmeric
- 1 tsp ground cinnamon
- small pinch of fresh grated ginger
- 1 tbsp coconut oil
- up to 1 tbsp honey (optional)
Directions
- Pour all the ingredients into a saucepan and heat until it lightly boils.
- Give it all a good whisk to combine.
- Serve hot in your favourite mug.
Aim for 1-2 cups per day.
Bone Broth
Bone broth is a rich source of collagen, a substance used for bone remodelling. It will be in high demand at this time and some studies have shown the protective impact of collagen on bone health. Beef bones are typically best.

Ingredients
- 400g fresh bones (beef/lamb/chicken, ask your butchers, they are usually very cheap!)
- 2 carrots, chopped
- 2 celery sticks, chopped
- 1 onion, chopped
- 1 tbsp cider vinegar
- Filtered water
Directions
- Firstly, if using beef or lamb bones, place in a roasting dish and roast in the oven for 30 minutes on 200’C as it helps to bring out the flavours.
- Place all ingredients into a deep pan and cover with filtered water so everything is covered. Bring to the boil and then leave to simmer with a lid on, on a low heat for up to 48 hours.
- If a film appears on the top then skim it off. The better quality the meat, the less amount of film will appear.
- Store in an air tight glass container in the fridge for up to 4-5 days, you can also freeze this.
If you cannot make it yourself, here is a company I discovered recently who have produced a great product – http://ossaorganic.com
Alternatively, if making or drinking broth isn’t your thing you can also use a hydrolyzed collagen formula.
Natto
This naturally fermented soy contains good levels of a specific vitamin K known as MK-7. This has been shown to help with bone calcification better than other forms of vitamin K.
3. Emphasize foods that are rich in bone supporting nutrients
Click the image below to download further information about the vitamin and minerals strongly associated with bone health and the foods rich in those nutrients. It is good to pay attention to these foods and include an array of those foods in your diet where possible.
4. Ensure adequate protein intake
Proteins have a number of functions when it comes to fracture recovery. Some of their main roles include:
Catalysts – Enzymes are proteins that are required for every function in the body.
Messengers – Hormones that act as chemical messengers that can help create an anabolic environment which can help improve the rate of tissue recovery. Cytokines are also proteins made by the immune cells and are crucial in the acute phase of fracture recovery.
Structural – Collagen is the main structural protein in connective tissue and is the most abundant tissue in mammals, making up around 25-35% of whole-body protein content.
Transporters – Movement and delivery of nutrients and waste products throughout the body.
Buffers – these can help maintain appropriate pH, accepting and/or donating hydrogen ions, allowing enzymes to function.
Following a fracture, our protein requirements increase to be able to support the above functions and allow for healing to take place. Healing requires the synthesis of new proteins from amino acids acquired from the foods we eat. Daily minimum requirements are around 0.8g per kg of body weight per day. Even for a healthy diet I believe that is low, and crucially during the healing phase an intake more like 1.2-1.8g per kg of your bodyweight would be advisable.
Because bone is a living tissue made up of protein in which mineral crystals are embedded, roughly half the bone is actually made up of protein. Under eating protein can lead to poor callus formation causing the bone to remain weaker for longer, which will generally cause more complications.
Even small increases in protein of 10-20g per day on top of previous levels have shown increased healing. Small increases can easily be made with increasing proteins naturally from food, and in some cases protein supplementation may be of benefit, particularly if following a vegan or vegetarian diet.
Check out the Fit For Films series of articles on protein to help you understand more about this subject and the best foods to help you reach your protein requirements.
- Protein: Understanding the importance and establishing your protein goal
- Protein: Debunking myths
- Protein: What should I eat?
5. Consider Supplemental Support
If you are able to nail down the basics of your diet, then adding additional nutrients whilst there is high demand during the repair process may also benefit the healing process.
Here are some supplement considerations that I might have when working with clients recovering from bone fractures, especially when someone has experienced multiple fractures.
Multivitamin and Mineral Complex
Ideally containing a form of calcium known as MCHC, which has been shown to enhance bone remodelling compared to more standard forms of calcium.
Vitamin D3 with K2
Vitamin K plays a central role in bone health and our ability to heal from a fracture quickly. Vitamin K synthesizes osteocalcin which is the bone matrix that calcium crystalises, and also aids in the binding of calcium to the bone matrix.
Vitamin D has gained a vast amount of popularity over recent years, and much research has taken place determining both functions and implications of vitamin D. Research has indicated it may be useful in preventing everything from osteoporosis to cardiovascular disease, cancer, autoimmunity and much more.
Research also suggests that around 40-50% of the population may be deficient in Vitamin D.
Vitamin C, ideally a liposomal form
Involved in collagen formation to assist bone remodelling and an important antioxidant. Liposomal forms provide the highest absorption levels, thus a lower dose is appropriate compared to other forms of vitamin C.
Hydrolysed Collagen
May help to support bone remodelling particularly with multiple fractures.
Additional Anti-inflammatory Support
If one is suffering with high levels of inflammation beyond the initial acute period of around 5 days post-accident or surgery, we recommend the inclusion of some anti-inflammatories.
Some of the best anti-inflammatories available are:
Curcumin – An extract typically from the spice turmeric.
Essential fatty acids – typically from fish oil, krill or algae oil. Fish oil is preferable because of the dosage levels that can be reached at still an affordable price comparative to krill and algae. Of course, if you are a strict vegan then the algae oil is better than no oil at all.
Other natural anti-inflammatories include Boswellia, proteolytic enzymes, pine bark/grapeseed extract.
Testimonials
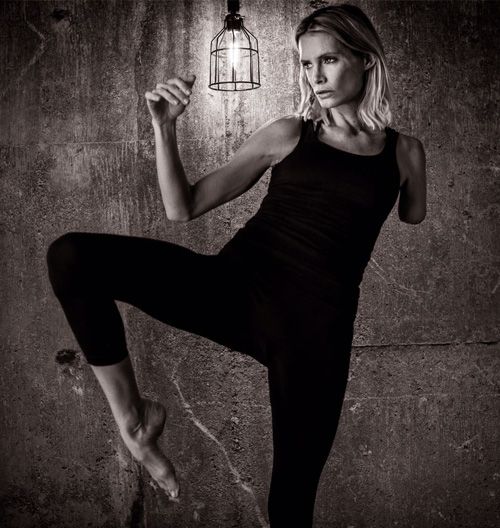
Olivia Jackson – Stunt Performer
“I’ve been on a bone protocol with Steve quite a few times now & had absolutely ground-breaking results. I once went in for a shoulder reconstruction, where they broke both my shoulder blade & collarbone, shifted them about & re-fixed. The surgeon said that due to the nature of my injuries it would take at least 6 months for the bones to heal 100% but when I returned for my check-up 6 weeks later & he did a CT scan to check the bones’ condition, he was absolutely astounded that they had healed 100% already”
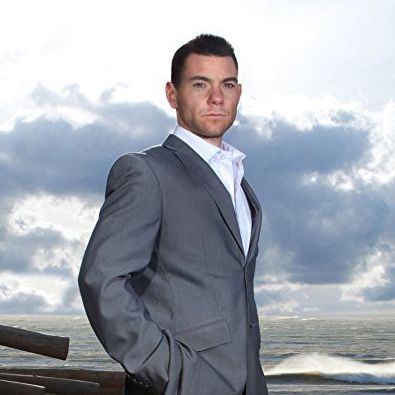
Andy Pilgrim - Stunt Performer
After multiple breaks in my tibia and fibula, having an operation where smashed up cartilage was removed from my ankle and 19 pins speared through my leg to scaffold my bones I knew pretty much straight away that the jam sandwiches on offer in the hospital ward weren’t going to get me fixed any time soon. I needed to get back to work and that would only happen after some serious bone growth… Enter Fit For Films who advised me on the best food choices for inflammation and healing and top quality supplement choices to speed up recovery. They were both empathetic and extremely knowledgeable to my case and I wouldn’t hesitate to use them again for any nutritional needs that I have.”



